During the month of June 2025, we had the honor of collaborating with Dr. Micun Micunovic in solving a major challenge: a patient with a skull bone defect needed reconstruction, but due to the specific configuration of the defect, no commercially available solution was ideal. After the problem was solved with excellent results, we spoke with Dr. Micunovic about the process, challenges, and outcome.
1. Can you briefly explain how this complicated case is special and what led you to decide on an individualized 3D-printed solution?
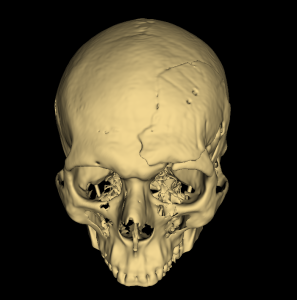
Dear colleagues, first let me acquaint you with the case briefly – it concerns a 26-year-old man who was severely injured in another country with involvement of multiple organ systems, including brain hemorrhage which was resolved by opening the head and “cleaning” the bleeding (epidural hematoma). After stabilizing the condition, he was transferred to our hospital “St. Erazmo” – Ohrid for continued treatment. Already at admission, he had an infection of the operative wound on the head, which despite antibiotic therapy developed into an infection of the bone “cap.” The only way to treat such an infection was removal of the bone “cap,” after which the wound healed properly, but as a consequence of the intervention, a hole remained on the left corner of the forehead, namely the left fronto-orbital region.
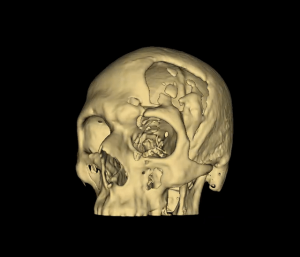

The “hole in the head” caused him psychological difficulties and he covered the defect by growing hair and constantly wearing a cap on his head. The only way to aesthetically and functionally solve the problem was cranioplasty, making a new bone cap to cover the defect. The cheapest and most effective correction for making “artificial bone” is using polymethylmethacrylate or medical biological cement (hereinafter referred to as cement). We have had other cases and although it’s not a common problem, mainly smaller bone defects of the skull we have made with cement shaped by manual “sculpting.” I thought that the specificity of the case required more than personal sculpting skills due to the hole on the visible part of the head, namely the use of technology in its manufacture. The intervention can be performed at least 6 months after sanitation of the infection provided there are no other parameters for possible infection in the patient. The work was postponed for 3 years while I was looking for a solution to the problem. One of the options was collaboration with dentist-implantologists who I saw in advertisements were using 3D printing, but the collaboration was not realized due to the inability to incorporate the computerized tomography scans of the patient’s head into their printers. Then, my colleague Dr. Ana Tomevska from our hospital mentioned the name of Dr. Stefan Arsenkov, an abdominal surgeon from the Surgical Hospital “St. Naum Ohridski” and I remembered that I had seen on television his presentation about the usefulness of 3D printing in surgery. I immediately contacted him, explained the problem, after which he enthusiastically and quickly found a solution to the problem and within two-three weeks made a mold that we would use to obtain an approximately perfect copy of the old discarded bone to cover the defect. The intervention was performed during June 2025 and went excellently in collaboration with Dr. Stefan Arsenkov, achieving the expected effect. The intervention proceeded without particular problems.
2. How did the use of our 3D-printed mold affect the way you planned and performed the surgery, compared to classical methods?
My superficial knowledge of 3D printing is that both a “positive” of the defect can be made, namely a modeled mold that can immediately be placed on the defect and a “negative,” namely molds that can be used with our cement to make a “positive.” We chose the cheaper variant, namely using a “negative” mold, a mold made from medical resin that supports sterilization. Intraoperatively, we shaped the “positive” with cement with which we covered the bone defect with some minimal corrections to it, which completely replaced the more expensive variant of direct printing of the positive. The mold, of course, the patient, despite the symbolic price, did not pay for it, it was paid by a sponsor. Classical methods involve manual making of the mold with cement during the operation. I was sure that with their use we would not even approximately make correct reconstruction. Therefore, I rejected the option “to try whether manual manufacturing would work.”


3. How did the intervention itself proceed? Did the implant fit well and integrate with the surrounding tissue?
Before the intervention, detailed planning of the skin incision on the scalp naturally precedes to obtain sufficiently exposed surface for reconstruction. This is done to avoid disrupting the vascularization of the scalp flap and the possibility to fully expose the edges of the bone defect for definitive integration of the new bone cap. In principle, when opening a bone cap is planned for primary head surgery, it is usually with straight edges and commonly with rectangular or similar polygonal shape. In this case, after removal of the infected bone flap, for three years while the patient awaited reconstruction, the edge of the bone defect was very irregular, especially at the base of the orbital bone. Namely, the outer layer of the hard covering of the brain has the potential to generate bone tissue (which is specific for small children with incomplete head growth, but also occurred in this patient at 23 years old) whereby there was a part of bone connected to the lower edge of the bone defect and islands of bone on the hard covering. The challenge in dissecting the soft tissue was especially with regard to the orbital muscle, because it was necessary to fully expose the free edges of the bone defect as well as the bone islands, while not causing injury to the hard covering of the brain (to avoid cerebrospinal fluid leakage, brain injury, bleeding…). In the part of dissection of the lower edge of the orbital bone defect, I had difficulties in orienting the bone edges. At the suggestion of Dr. Arsenkov, directly in front of me he held the printed plastic model of the bone defect which guided me and made it easier for faster orientation of the irregular free edges of the bone defect.


After all free straight and irregular edges of the entire bone defect were prepared, the second phase of the intervention followed, where we gave the honor to Dr. Stefan Arsenkov to make the “positive” from medical cement using the previously detailed printed sterile 3D mold onto which the cement was poured and waited for it to harden. With the help of an electric drill, corrections were made to the edges of the new bone cap and completely perfectly congruent fitting of the bone cap and covering of the defect was obtained. When exposing the operative field, the opposite side of the fronto-orbital region was also visible and they were symmetrical as in a mirror.

4. What were the results – both from functional and aesthetic aspects?
Unwanted effects of lack of bone cap on the scalp can be aesthetic and psychological difficulties and the possibility of “open head syndrome,” namely functional neurological impairment such as general weakness, fatigue, nausea, motor weakness, cognitive impairments, speech problems. The current patient only suffered from the aesthetic deficiency of bone or “hole” on the forehead which he covered by growing hair and regularly using a cap and was often exposed to social isolation from the environment due to that deficiency.
5. From your perspective, how much is this individual approach more precise and efficient compared to standard reconstruction techniques?
Standard cranioplasty techniques using medical cement shaped by hand, I believe that even a surgeon with the greatest sense of aesthetics and sculpting would not even approximately achieve the effect as with technologically assisted 3D printing of models with appropriate software.


6. What reactions did the patient have – both to the process itself and to the final result?
The patient from the very beginning was informed that we want to achieve close to ideal reconstruction of the bone defect, that we had consulted with experts in the field of 3D printing. The procedure for making the frontal bone cap was completely explained to him, to which he agreed. With the final result, the patient is satisfied, not expecting that such good correction of the bone defect could be achieved.
7. Did and how did this case change your approach to other complex cranioplasty cases?
Cranioplasty is a procedure that should follow a previously performed craniectomy, namely discarded bone. Bone removal can be performed with high intracranial pressure that cannot be controlled, infection of the bone cap, damage to the bone cap from tumor growth in primary or secondary involvement. Although cranioplasties in our practice are not frequent as interventions, certainly, after this positive experience, every cranioplasty that would involve part of a defect in the skull base, frontal, orbital region, frontal sinuses, would be planned with some form of 3D printing.
8. What would you recommend to your neurosurgeon colleagues who are considering incorporating 3D printing into their practice?
I would encourage them to use this type of assisted surgical planning, as it can help in other problems besides cranioplasties.
9. In what other situations in neurosurgery do you see potential for using 3D-printed, individualized solutions?
3D printing can help in preoperative manufacturing and reconstruction of brain blood vessels in case of aneurysm (a blister on the wall of a blood vessel that represents a life-threatening condition when it ruptures). For exclusion of aneurysms, relations with surrounding blood vessels are important, orientation, planning of head opening, dissection of arachnoid covering and trabeculae, position of inflow and outflow blood vessels in relation to aneurysms, and similar. Another use, printing of tumors, especially those connected to the hard brain covering and relation to blood vessels around the tumor that must be protected, which would guide the surgeon for easier orientation and preservation of the same. Regarding spinal surgery which is a borderline specialty of neurosurgeons, traumatologists, orthopedists, it can help in planning correction of bone defects, solving fractures, orientation of transpedicular screws, orientation of derotated vertebrae, planning osteotomies of vertebrae, and similar.
10. What does this case show, in your opinion, about the future of personalized medicine in neurosurgery?
This type of 3D printing use is not at all new in the world and has been performed 1-2 decades ago in developed countries. It was our honor to meet an enthusiast like Dr. Stefan Arsenkov who quickly understood the problem and rapidly realized the solution. In our joint collaboration, we saw excellent effects in treatment. If we are offered similar problems of bone defects, tumors for which we would like to know the relation to parts of calvaria bones or skull base or relationship to vital blood vessels, we would certainly again seek collaboration. I recommend to my neurosurgeon colleagues to start using 3D printing with which they will see improvement in precision in their work, improvement in self-confidence at work, and reduction in fear of unpredictable surprises.



